
It’s essential to have an efficient system for tracking payments, following QuickBooks up on unpaid bills and resolving any discrepancies that may arise. This requires substantial time and resources, which can be difficult to come by in a busy practice. The tips discussed above for improving your accounts receivables provide a solid foundation for improved A/R management.
Understanding Codes: ICD, CPT, and HCPCS

Automating your end-to-end workflow will significantly reduce errors such as duplicate payments, over-payments, fraudulent payments, and more. What was once a frustrating, labor-intensive, and costly task for already overburdened AR teams can become a valuable part of the process that boosts your competitive edge. An automated AR system allows accounts receivable officers to keep track of payments and track bills as they near their due date. This enables AR offices to send out reminders, when necessary, and stay on top of customers who are becoming potential credit risks. This is another situation where manual processes and out-of-date systems can cause significant problems.
Bridging the Gaps: Strengthening Communication and Transparency in Medical Billing Partnerships
This information is crucial in selecting the right plan that aligns with your healthcare needs and budget. Understanding the nuances of each type can help you make an informed decision when choosing your insurance coverage. This knowledge is key to ensuring you have access to the care you need while managing costs effectively. The HCFA 1500 form use most often by the healthcare industry for medical billing and insurance claims submissions. Officially it is now referred to as the CMS-1500 form, though in conversation between professionals about the form, you may still hear it referred to as the HCFA 1500 form due its historic use. (HCFA) — the predecessor agency now known as the Centers for Medicare & Medicaid Services (CMS) — first developed this form.
Patient Dissatisfaction

In a highly regulated industry such as healthcare, compliance violations can be incredibly accounts receivable in healthcare damaging. Not only does noncompliance lead to fines, sanctions, and accreditation issues, it also does lasting damage to an organization’s reputation and brand. Automating accounts receivable processes is the surest way to avoid compliance errors involving data privacy, invoicing practices, accounting fraud, and other key areas of concern. Patients need to know that their healthcare provider can be trusted not only with their health, but also their payments and privacy.
The doctor acts as the member’s regular physician and coordinates any other care the member needs, such as a visit to a specialist or hospitalization. Level II is for products, supplies and services not otherwise included (ambulance services, DME, prosthetics, orthotics or supplies used outside a doctor’s office). RARCs provide additional explanations for an adjustment already described by a CARC (supplemental RARCs) or convey information about remittance processing (informational RARCs or Alerts). Centers for Medicare & Medicaid Services (CMS) – Stay updated on the latest regulations for Medicare and Medicaid billing.
How Accounts Receivable (AR) Services Improve Healthcare Revenue Cycle
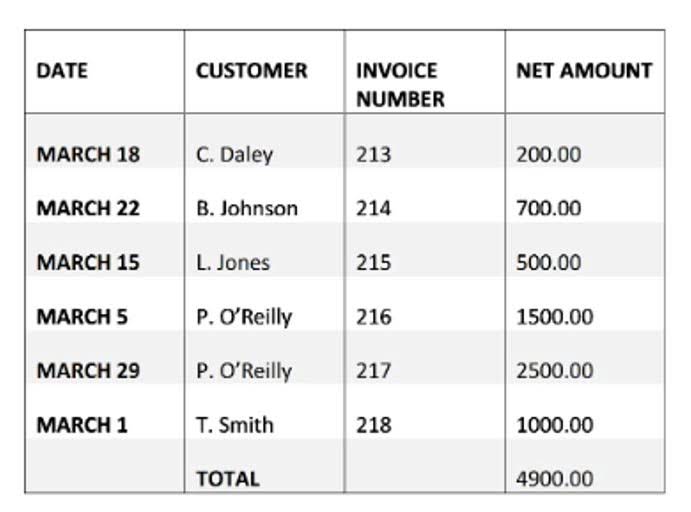
Done effectively and consistently, AR follow-up will shorten the AR cycle and prevent bad debt. Accounts Receivable in medical billing is far more than just a number on a spreadsheet it’s a reflection of your organization’s financial health and billing efficiency. Bookkeeping 101 Accounts Receivable (AR) in medical billing refers to the outstanding amount of money a healthcare provider is owed for services already delivered but not yet paid for.
- When an insurance provider contacts another to see if they’re currently providing specific coverage.
- You can collect more money faster by collecting patient payments upfront, offering financing options, and providing patient estimates.
- As a result, medical practices can reduce AR, and patients remain stress-free simultaneously.
- The medical provider receives payment from this source for all doctor services including appointments visits and therapeutic procedures.
Managing Your Healthcare Accounts Receivable Process and Improving Patient Communications

UB-04 is a standardized form used in hospital billing to ensure consistency in claims submission. Getting prior authorizations for services that are not covered under the plan can save you a lot of hassle and time. Make sure that you get authorization from the insurer before you provide any such service.
Best Practices for Effective AR Management
Tracking AR days in medical billing is crucial to prevent revenue loss and ensure timely collections. Moreover, it also helps you identify the potential bottlenecks and gaps in your billing cycle. So, what causes high AR for some practices while others enjoy timely payment collections from both the payors and the patients? Clearly, AR in medical billing presents several challenges to healthcare providers’ financial wellness and overall growth. In an effort to maintain a clean accounts receivable balance, healthcare providers may write off certain outstanding balances. A healthcare provider has exhausted all efforts to collect payment from a patient who owes $500.
